1. Who does the Mental Health Act 1983 apply to?
The Mental Health Act 1983 (MHA), which was amended in 2007, provides ways of assessing, treating and caring for people who have a serious mental disorder that puts them or other people at risk. It sets out when:
- people with mental disorders can be detained in hospital for assessment or treatment;
- people who are detained can be given treatment for their mental disorder without their consent (it also sets out the safeguards people must get in this situation); and
- people with mental disorders can be made subject to guardianship or aftercare, under supervision to protect them or other people.
Most of the MHA does not distinguish between people who have the mental capacity to make decisions and those who do not. Many people covered by the MHA have the mental capacity to make decisions for themselves.
Decision makers will need to decide whether to use either the MHA or Mental Capacity Act (MCA) to meet the needs of people with mental health problems who lack capacity to make decisions about their own treatment. Where someone with a mental health disorder is subject to a Community Treatment Order (CTO) or Guardianship under the MHA, and lacks capacity, they may have a Deprivation of Liberty Safeguards in place. Otherwise a person cannot be subject to the two frameworks at the same time.
Click here to view flowchart: Deciding whether the MHA and /or MCA can be used.
2. What are the Limits of the Mental Capacity Act?
The MCA provides legal protection for people who are caring for or treating a person who lacks mental capacity. But the principles of the MCA must be followed (see Principles, Mental Capacity) and action can only be taken if it is in the person’s best interests. This applies to care or treatment for physical and mental conditions, and can apply to treatment for people with mental disorders, however serious those disorders are.
The MCA does have its limits, for example a practitioner who is restraining an adult in their care only has protection if the restraint is:
- necessary to protect the person who lacks capacity from harm; and
- in proportion to the likelihood and seriousness of that harm.
The Deprivation of Liberty Safeguards (DoLS) provides safeguards for people who lack the mental capacity specifically to consent to treatment or care in either a hospital or registered care home that amounts to a deprivation of liberty, and detention under the MHA is not appropriate for them at that time. See also Deprivation of Liberty Safeguards chapter.
The MCA also does not allow for treatment to be given if it goes against a valid and applicable advance decision to refuse treatment (see Advance Care Planning chapter).
None of these restrictions apply to treatment for mental disorder given under the MHA – but other restrictions do.
3. When can a Person be Detained under the MHA?
A person can be detained for assessment under section 2 MHA if both of the following criteria apply:
- the person is suffering from a mental disorder of a nature or degree which warrants their detention in hospital for assessment (or for assessment followed by treatment) for at least a limited period; and
- the person ought to be so detained in the interests of their own health or safety or with a view to the protection of others.
A person can be detained for treatment under section 3 MHA if all the following criteria apply:
- the person is suffering from a mental disorder of a nature or degree which makes it appropriate for them to receive medical treatment in hospital;
- it is necessary for the health or safety of the person or for the protection of other persons that they should receive such treatment and it cannot be provided unless the patient is detained under this section; and
- appropriate medical treatment is available.
Decision makers should consider using the MHA if they are not sure it will be possible, or sufficient, to rely on the MCA. They do not have to ask the Court of Protection to rule that the MCA does not apply before using the MHA.
If a clinician believes that they can safely assess or treat a person under the MCA, they do not need to consider using the MHA. In this situation, it would be difficult to meet the requirements of the MHA anyway. Certain serious treatments under the MCA, such as non-therapeutic sterilisation or withdrawal of artificial hydration or ventilation, must be referred to the Court of Protection for a final decision. Furthermore, a person should not be treated for a mental disorder or on a psychiatric ward under DoLS if they are likely to be treatable under the MHA.
A person cannot be treated under the MHA unless they meet the relevant criteria for being detained.
4. How does the MCA apply to a Patient subject to Guardianship under the MHA?
Guardianship gives someone (usually a local authority social care department) the exclusive right to decide where a person should live – but in doing so they cannot deprive the person of their liberty (see Deprivation of Liberty Safeguards). The guardian can also require the person to attend for treatment, work, training or education at specific times and places, and they can demand that a doctor, approved social worker or another relevant person have access to the person wherever they live. Guardianship can apply whether or not the person has the mental capacity to make decisions about care and treatment. It does not give anyone the right to treat the person without their permission or to consent to treatment on their behalf.
Decision makers must never consider guardianship as a way to avoid applying the MCA.
5. Community Treatment Orders
A Community Treatment Order (CTO) is used where it is necessary for the patient’s health or safety or for the protection of others to continue to receive treatment after their discharge from hospital. It seeks to prevent the ‘revolving door’ scenario and the harm which could arise from relapse.
A key feature of the CTO framework is that it is suitable only where there is no reason to think that the patient will need further treatment as a detained in-patient for the time being, but where the responsible clinician needs to be able to recall the patient to hospital if necessary.
5.1 Deprivation of liberty while on a CTO, leave or subject to guardianship
Patients who are on a CTO or on leave, and who lack capacity to consent to the arrangements required for their care or treatment, may occasionally need to be detained for further care or treatment for their mental disorder in circumstances in which recall to hospital for this purpose is not considered necessary. They might also need to be admitted to a care home or hospital because of physical health problems.
If the person is to be detained in a registered care home, a DoLS authorisation must be obtained. A deprivation of liberty can exist alongside a CTO or leave of absence, as long as there is no conflict with the conditions of the CTO or leave set by the patient’s responsible clinician.
If the person is to be detained in a hospital for further treatment for mental disorder (whether or not they will also receive treatment for physical health problems), they should be recalled so they can be treated under the MHA. The MCA cannot be used to authorise the deprivation of their liberty.
6. How does the Mental Capacity Act affect People covered by the Mental Health Act?
There is no reason to assume a person lacks mental capacity to make their own decisions just because they are subject under the MHA to:
- detention;
- guardianship; or
- after-care under supervision.
People who lack mental capacity to make specific decisions are still protected by the MCA even if they are subject to the MHA (this includes people who are subject to the MHA as a result of court proceedings). But there are four important exceptions:
- if a person is liable to be detained under the MHA, decision makers cannot normally rely on the MCA to give mental health treatment or make decisions about that treatment on someone’s behalf;
- if a person can be given mental health treatment without their consent because they are liable to be detained under the MHA, they can also be given mental health treatment that goes against an advance decision to refuse treatment;
- if a person is subject to guardianship, the guardian has the exclusive right to take certain decisions, including where the person is to live; and
- Independent Mental Capacity Advocates (IMCAs) do not have to be involved in decisions about serious medical treatment or accommodation, if the decisions are made under the MHA (see Independent Mental Capacity Advocacy Service chapter).
7. What are the Implications for People who need Treatment for a Mental Disorder?
Under the MHA, subject to certain conditions, doctors can give treatment for mental disorders to detained patients without their consent – whether or not they have the mental capacity to give that consent.
Where Part 4 of the MHA applies, the MCA cannot be used to give medical treatment for a mental disorder to patients who lack mental capacity to consent. Nor can anyone else, like an attorney or a deputy, use the MCA to give consent for that treatment. This is because Part 4 of the MHA already allows clinicians, if they comply with the relevant rules, to give patients medical treatment for mental disorder even though they lack the capacity to consent. In this context, medical treatment includes nursing and care, habilitation and rehabilitation under medical supervision.
However, clinicians treating people for mental disorder under the MHA cannot simply ignore a person’s mental capacity to consent to treatment. As a matter of good practice (and in some cases in order to comply with the MHA) they will always need to assess and record:
- whether patients have mental capacity to consent to treatment, and
- if so, whether they have consented to or refused that treatment.
8. How does the Mental Health Act affect Advance Decisions to Refuse Treatment?
See also Advance Decisions to Refuse Treatment, Advance Care Planning chapter
The MHA does not affect a person’s advance decision to refuse treatment, unless the person can be treated for mental disorder without their consent. In this situation healthcare staff can treat patients for their mental disorder, even if they have made an advance decision to refuse such treatment.
But even then healthcare staff must consider a valid and applicable advance decision to refuse treatment as they would a decision made by a person with capacity at the time they are asked to consent to treatment. For example, they should consider whether they could use a different type of treatment which the patient has not refused in advance. If healthcare staff do not follow an advance decision, they should record this in the patient’s notes with reasons.
Even if a patient is being treated without their consent under Part 4 of the MHA, an advance decision to refuse other forms of treatment is still valid. Being subject to guardianship or aftercare under supervision does not affect an advance decision in any way.
9. Does the MHA affect the Duties of Attorneys and Deputies?
In general, the MHA does not affect the powers of attorneys and deputies. But there are two exceptions:
- they will not be able to give consent on a patient’s behalf for treatment under Part 4 of the MHA, where the patient is liable to be detained under the Act; and
- they will not be able to take decisions:
- about where a person subject to guardianship should live, or
- that conflict with decisions that a guardian has a legal right to make.
Being subject to the MHA does not stop patients creating new Lasting Powers of Attorney (if they have the mental capacity to do so), or does it stop the Court of Protection from appointing a deputy for them.
Attorneys and deputies are able to exercise patients’ rights under the MHA, if they have the relevant authority. In particular, some personal health and welfare attorneys and deputies may be able to apply to the First Tier Tribunal for the patient’s discharge from detention, guardianship or aftercare under supervision.
The MHA also gives various rights to a patient’s nearest relative (see MCA Code of Practice for further information).
Clinicians and others involved in the assessment or treatment of patients under the MHA should try to find out if the person has an attorney or deputy.
10. Does the MHA affect when Independent Mental Capacity Advocates must be instructed?
10.1 Independent Mental Capacity Advocates
See also Independent Mental Capacity Advocacy Service chapter
There is no duty to instruct an IMCA for decisions about serious medical treatment which is being provided under the MHA. Nor is there a duty to do so in respect of a move into accommodation, or a change of accommodation, if the person is required to live there because of an obligation under the MHA.
However, the rules for instructing an IMCA for patients subject to the MHA who may need serious medical treatment not related to their mental disorder are the same as for any other patient.
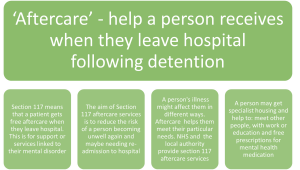
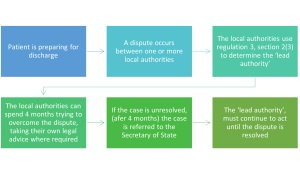
The duty to instruct an IMCA would also apply if accommodation is being planned as part of the aftercare under section 117 of the MHA following the person’s discharge (see 117 Aftercare chapter).
10.2 Independent Mental Health Advocates
Independent mental health advocacy services provide an additional safeguard for patients who are subject to the MHA. Independent Mental Health Advocates (IMHAs) are specialist advocates who are trained to work within the framework of the Act and enable patients to participate in decision-making, for example by encouraging them to express their views and supporting them to communicate their views. IMHAs should be independent of any person who has been professionally involved in the patient’s medical treatment.
IMHA services do not replace any other advocacy and support services that are available to patients, such as independent mental capacity advocates (IMCAs) or representatives for patients who lack mental capacity, and should work alongside these services.
11. Further Reading
11.1 Relevant chapters
Deprivation of Liberty Safeguards
11.2 Relevant information
Mental Capacity Act 2005 Code of Practice (2007)
Mental Health Act 1983: Code of Practice (2015)